Urinary catheter insertion is a common procedure for managing urinary complications in residential aged care facilities (RACFs). Research, however, suggests that catheter-associated urinary tract infections are the most common nosocomial infections worldwide. Of healthcare-associated urinary tract infections, 80% occur in catheterised patients (Gesmundo, 2016 & Gilbert et al., 2018).
The National Ageing Research Institute (2024) estimates that 5-8% of people living in RACFs have an indwelling catheter. This prevalence is influenced by factors such as the resident population’s health conditions, facility practices, and the availability of alternative management strategies for urinary incontinence.
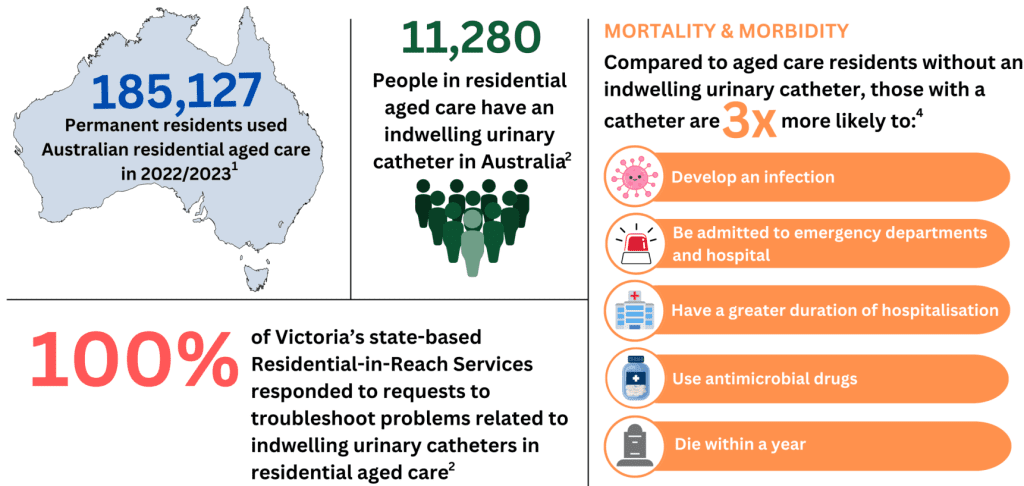
Image source: National Ageing Research Institute 2024
The problem
In RACFs, off-site physicians rely heavily on inexperienced direct-care clinical staff to assess residents for possible complications. However, the aged care workforce is often understaffed and undertrained, and efforts to educate are often hampered by high staff turnover and a lack of local resources (Crnich et al., 2017; Dyer et al., 2015; Royal Commission into Aged Care Quality and Safety, 2021). This often leads to unnecessary transfers to hospital, particularly after hours, placing additional burden on the public health system and causing distress for the aged care resident.
Factors contributing to urinary catheter complications
In aged care facilities, the complications associated with urinary catheters are a significant concern. While exact statistics can vary, the most reported complications include:
- Urinary tract infections (UTIs)
UTIs are among the most common complications associated with urinary catheters. The prevalence of UTIs in aged care facilities can be influenced by factors like catheter care practices and resident health. - Catheter-associated bloodstream infections (CABSI)
Although less common than UTIs, CABSI is a serious complication. The incidence is lower but still a notable concern in aged care settings. - Bladder and kidney damage
Long-term catheter use can potentially lead to bladder or kidney damage due to constant irritation or infection. - Catheter blockage and encrustation
Blockages due to sediment or encrustation can occur, leading to discomfort and potential complications. Regular monitoring and management are necessary to mitigate this risk. - Urethral injury
Improper catheterisation or prolonged use can lead to urethral trauma or injury. - Quality of life issues
Complications from catheters can also impact the overall quality of life for residents, including discomfort, reduced mobility, and social isolation.
These complications have been documented in several studies (Davis et al., 2020; Czwikla et al., 2023).
Addressing the problem
Nurses are leaders in health care and are well-placed to lead the prevention of catheter-related complications in RACFs (Wu et al., 2020). Nurses in RACFs can contribute to preventing deterioration for residents by providing quality catheter care. Quality care includes:
- Adhering to sterile techniques
Use sterile equipment and follow strict hand hygiene protocols during catheter insertion and maintenance to prevent infections. - Ensuring appropriate indication for catheter use
Use urinary catheters only when absolutely necessary and consider other management strategies for incontinence or urinary retention first. - Regular monitoring and care
Perform routine assessments of the catheter and insertion site, checking regularly for signs of infection, blockages, or other complications. - Maintaining catheter hygiene
Clean the catheter and surrounding area daily with mild soap and water. - Ensuring proper catheter maintenance
Keep the catheter and drainage bag below the level of the bladder to prevent backflow of urine and reduce the risk of infection. Regularly empty the drainage bag and ensure it is properly secured to avoid tugging or pulling on the catheter. - Educating residents and staff
Provide education on the importance of catheter care and the signs of complications. Train staff on proper catheter insertion and maintenance techniques.
Want to learn more?
To learn more about managing residents with urinary catheters in RACFs and what nurses can do to make a difference, The Australian College of Nursing (ACN) has developed an online learning course, Urinary Catheterisation. This course provides learners with evidence-based knowledge on risk prevention and reduction, management of problems associated with urinary catheterisation procedures and appropriate urinary catheter maintenance and care.
ACN also runs a regular Urinary Catheterisation face-to-face course. This course equips nurses with the theoretical and clinical skills required to perform safe and effective urinary and suprapubic catheterisation in accordance with evidence-based guidelines and within scope of practice. This knowledge and skill will ensure both the protection of patients receiving the procedure and the delivery of high standards of nursing care. Upcoming course dates and venues can be found here.
Author: Judith Smith
Director of Professional Development (ACN)
Judith Smith is the Director of Professional Development at the Australian College of Nursing. In addition to being the primary figure overseeing the Aged Care Transition to Practice Program, Judith leads several other national nursing initiatives through ACN. Her passion lies in enhancing the capacity of the nursing workforce by actively engaging nurses across all levels. Judith’s approach involves challenging and empowering nurses to achieve professional and personal growth, enabling them to emerge as leaders in their field. This commitment is evident in her successful career, which has spanned nursing education and clinical, tertiary, and corporate settings.
Beyond her role, Judith has contributed nationally and internationally to curriculum design. She actively participates in state and national working parties and advisory groups to enhance service performance and patient outcomes. Judith’s influence extends to her contributions to various publications, including peer-reviewed journals and as a chapter author in professional textbooks.

References
Czwikla, J., Wandscher, K., Helbach, J., Fassmer, A., Schmiemann, G., & Hoffmann, F. (2023). Prevalence of indwelling urinary catheters in nursing home residents: Systematic review. International Journal of Nursing Studies, 145. https://doi.org/10.1016/j.ijnurstu.2023.104555
Crnich, C., Jump, R., & Nace, D. (2017). Improving management of urinary tract infections in older adults: A paradigm shift or therapeutic nihilism? J Am Geriatr Soc, 65(8), 1661–63. https://doi.org/10.1111/jgs.14961
Davis, N. F., Bhatt, N. R., & MacCraith, E. et al. (2020). Long-term outcomes of urethral catheterisation injuries: a prospective multi-institutional study. World Journal of Urology, 38, 473–480.
Dyar, J., Pagani, L., & Pulcini, C. (2015). Strategies and challenges of antimicrobial stewardship in long-term care facilities. Clin Microbiol Infect, 21(1), 10–19. https://doi.org/10.1016/j.cmi.2014.09.005
Gesmundo, M. (2016). Enhancing nurses’ knowledge on catheter-associated urinary tract infection (CAUTI) prevention. Kai Tiaki Nursing Research, 7(1), 32-40.
Gilbert, B., Naidoo, T., & Redwig, F. (2018). Ins and Outs of Urinary Catheters. AJGP, 47(3), 132-136.
Lim, L., & Bennett, N. (2022). Improving management of urinary tract infections in residential aged care facilities. Australian Journal of General Practice, 51(8).
Ostaszkiewicz, J., Batchelor, F., Gilbert, C., & Cecil, J. et al. (2024). A consultation to inform a targeted response to catheter-associated care and complications in Victorian residential aged care homes. National Ageing Research Institute (NARI), March 2024.
Royal Commission into Aged Care Quality and Safety. (2021). Final report: Care, dignity and respect. Canberra, ACT: RCACQS.
Wu, M., Pu, L., Grealish, L., Jones, C., & Moyle, W. (2020). The effectiveness of nurse-led interventions for preventing urinary tract infections in older adults in residential aged care facilities: A systematic review. Journal of Clinical Nursing, 29(9), 1432-1444.





